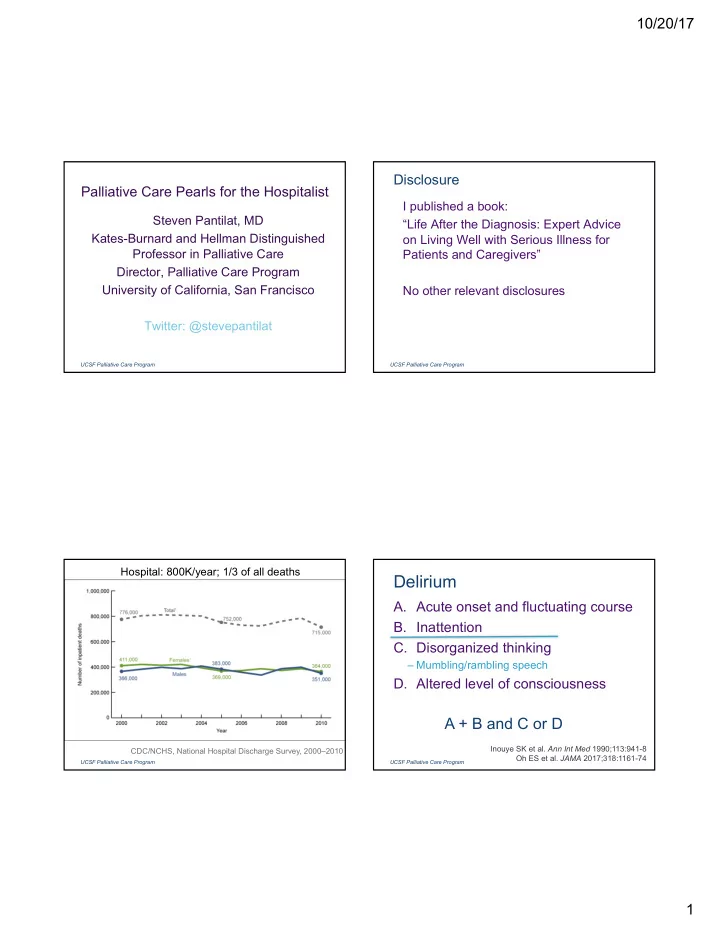
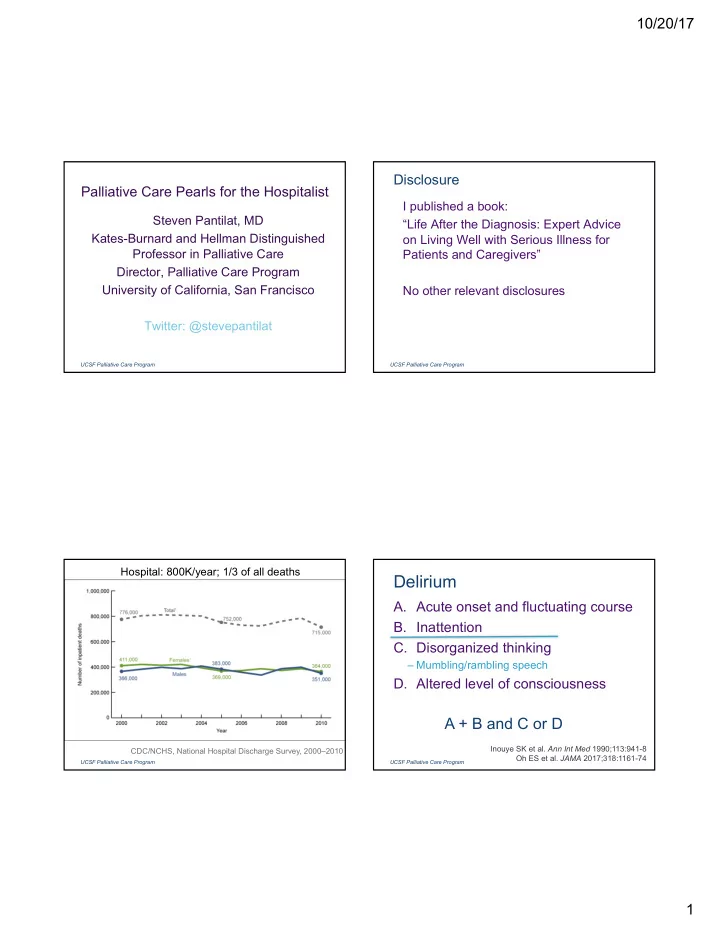
10/20/17 Disclosure Palliative Care Pearls for the Hospitalist I published a book: Steven Pantilat, MD “Life After the Diagnosis: Expert Advice Kates-Burnard and Hellman Distinguished on Living Well with Serious Illness for Professor in Palliative Care Patients and Caregivers” Director, Palliative Care Program University of California, San Francisco No other relevant disclosures Twitter: @stevepantilat UCSF Palliative Care Program UCSF Palliative Care Program Hospital: 800K/year; 1/3 of all deaths Delirium A. Acute onset and fluctuating course B. Inattention C. Disorganized thinking – Mumbling/rambling speech D. Altered level of consciousness A + B and C or D Inouye SK et al. Ann Int Med 1990;113:941-8 CDC/NCHS, National Hospital Discharge Survey, 2000–2010 Oh ES et al. JAMA 2017;318:1161-74 UCSF Palliative Care Program UCSF Palliative Care Program 1
10/20/17 Delirium at the End of Life +4 combative Very distressing +3 very agitated +2 agitated 80% +1 restless Delirium 0 alert and calm Hypoactive 80% RASS scale -1 drowsy -2 light sedation Hyperactive 20% -3 moderate sedation -4 deep sedation Dying -5 unarousable Hosie A et al. Pall Med 2013;27:486-98 UCSF Palliative Care Program UCSF Palliative Care Program Delirium: DDx Delirium: Prevention • Medications • Orientation – Anticholinergics, Steroids, Benzodiazepines, – Family/friends at bedside Opioids • Minimize immobilizing interventions • Pain – Oxygen, IV, suction • Infection • Calming • Metabolic derangements – Relaxation podcasts, music • Constipation/urinary retention – Massage – Reduce noise – Minimize awakenings Vidal M and Bruera E in Hospital-Based Palliative Medicine Pantilat, Anderson, Gonzales, Widera eds. Wiley Blackwell 2015 Hshieh TT et al. JAMA IM 2015;175:512-520 UCSF Palliative Care Program UCSF Palliative Care Program 2
10/20/17 Risperidone, Haloperidol or Placebo RCT Risperidone, Haloperidol or Placebo RCT • 247 palliative care inpatients with delirium • Delirium scores • 75 yo; 72% with cancer; PPS 40 – Risperidone worse than placebo every day – Haloperidol worse than placebo every day • 0.5mg orally q12hrs, up to 4mg/d • Midazolam use – Half dose for pts >65yo – Fewer placebo patients rescued (17% vs 34%) • Rescue: midazolam 2.5mg sq q2hrs • Median survival • Delirium scores every 8 hours – Placebo: 26 days • Outcome: Average of last 2 delirium scores – Risperidone: 17 days on day 3 – Haloperidol: 16 days Agar MR et al. JAMA IM 2017;177:34-42 Agar MR et al. JAMA IM 2017;177:34-42 UCSF Palliative Care Program UCSF Palliative Care Program Haloperidol + Lorazepam vs Haloperidol Haloperidol + Lorazepam vs Haloperidol Alone for Agitated Delirium Alone for Agitated Delirium • 90 palliative care unit patients with cancer • Median survival 73 hrs; 72% died with hyperactive delirium (RASS ≥ 2 in past • Greater reduction in RASS for haloperidol + 24hrs) lorazepam • 62 yo; most with Karnofsky ≤ 30 • Absolute RASS at 8hrs • Haloperidol 2mg IV q4hrs and 2mg q1hr prn – Haloperidol + lorazepam: -2.5 • RASS score q2hrs; if RASS ≥ 2: – Haloperidol : -0.7 • Haloperidol + lorazepam more likely to be –Lorazepam 3mg IV or placebo assessed by caregiver as comfortable (84% • Outcome: RASS score at 8hrs after vs 37%) lorazepam Hui Det al. JAMA 2017;318:1047-56 Hui Det al. JAMA 2017;318:1047-56 UCSF Palliative Care Program UCSF Palliative Care Program 3
10/20/17 Treatment of Delirium at the End of Life Hours prior to death Signs of Imminent Death mean/median (SD) • Little evidence of benefit of haloperidol Death rattle 57/23 (82) • Evidence of harm with benzodiazepines Respirations with • Assess for treatable causes 8/3 (18) mandibular movement – Pain, constipation, urinary retention Cyanosis of extremities 5/1 (11) • Use nonpharmacologic approaches Thready / no radial pulse 3/1 (4) • For severe, persistent agitation in the dying Swelling of hands patient, try haloperidol Cheyne-stokes breathing Pauses in breathing Give placebo Agonal breathing Morita T et al. Am J Hosp Pall Care 1998:Jul-Aug:217-22 Neufeld KJ et al. JAGS 2016;64:705-14 Oh ES et al. JAMA 2017;318:1161-74 UCSF Palliative Care Program UCSF Palliative Care Program Helping Loved Ones Helping Loved Ones • Support family and friends • Offer ideas about how to help • Wet mouth and lips • Children • Massage • Spirituality: “Are there any traditions in • Hold hands your family we should be aware of?” • Anticipate issues • Help achieve closure • Can she hear me? • Tell stories • Being present at the time of death • “ Forgive me, I forgive you, thank you, I • How will we know? love you, good-bye” UCSF Palliative Care Program UCSF Palliative Care Program 4
10/20/17 Prepare Loved Ones Moment of Death • Explain signs • How will we know? – Body shutting down – “ She will stop breathing ” • Offer prognosis • Death is not an emergency – Hours to days – Notify nurse when you are ready • Anticipate surprise – Can stay with your loved one as long as – “ May happen suddenly ” you need – “ She may wait to be alone to die because it may be too hard to leave you or because she may not want to burden you with it ” UCSF Palliative Care Program UCSF Palliative Care Program Resource for Palliative Care Info Helping Loved Ones After the Death • Next steps – “We will take care of her” Fast Facts – “You just need to choose a funeral home” https://www.mypcnow.org/fast-facts • Request an autopsy • Make a phone call Palliative Care Fast Facts app • Answer questions • Alleviate guilt • Send a card UCSF Palliative Care Program UCSF Palliative Care Program 5
10/20/17 There is no good death The goal is to live a good life UCSF Palliative Care Program UCSF Palliative Care Program Life After the Diagnosis • You can live well and long with serious illness –Palliative care can help you do both • Talk about what you hope for –It will encourage and nurture it • The goal is to live a good life in the face of serious illness UCSF Palliative Care Program UCSF Palliative Care Program 6
10/20/17 UCSF Palliative Care Program 7
Recommend
More recommend