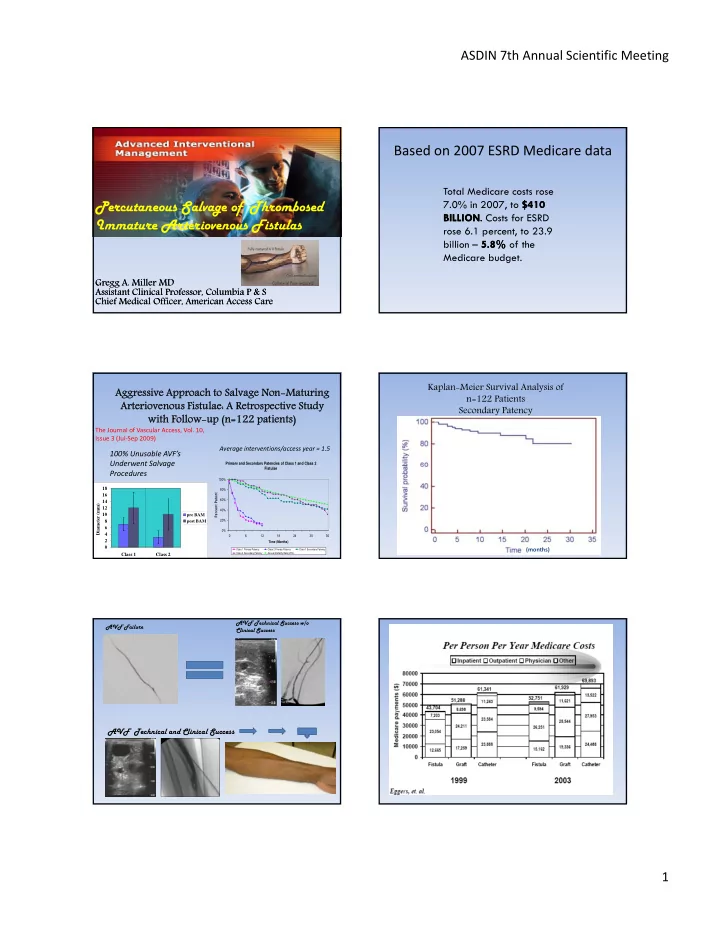
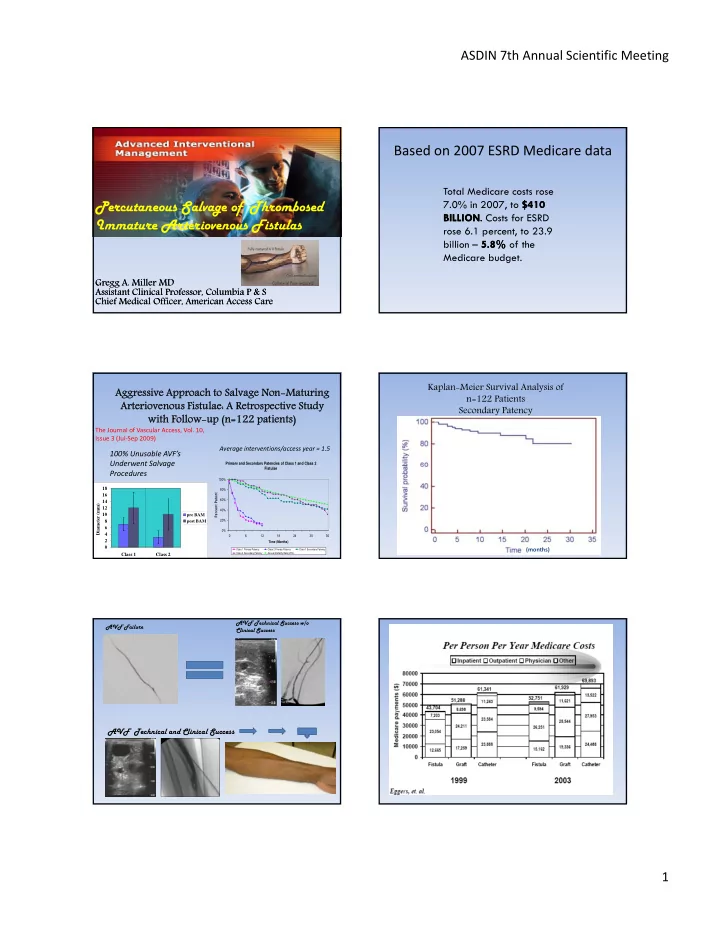
ASDIN 7th Annual Scientific Meeting Based on 2007 ESRD Medicare data Total Medicare costs rose Percutaneous Salvage of Thrombosed 7.0% in 2007, to $410 $410 BILLION BILLION BILLION . BILLION . . Costs for ESRD . Costs for ESRD Immature Arteriovenous Fistulas I A F l rose 6.1 percent, to 23.9 billion – 5.8% 5.8% of the Medicare budget. Gregg A. Miller MD Gregg A. Miller MD Assistant Clinical Professor, Columbia P & S Assistant Clinical Professor, Columbia P & S Chief Medical Officer, American Access Care Chief Medical Officer, American Access Care Kaplan-Meier Survival Analysis of Aggres Aggressiv sive Approach Approach to to Salvage Salvage Non-Maturing Non-Maturing n=122 Patients Arteriovenous Arteriovenous Fistulae: A istulae: A Retrospect Retrospective Study ive Study Secondary Patency with Follow-up with Follow-up (n=122 patients) (n=122 patients) The Journal of Vascular Access, Vol. 10, Issue 3 (Jul ‐ Sep 2009) Average interventions/access year = 1.5 100% Unusable AVF’s Underwent Salvage Underwent Salvage Primary and Secondary Patencies of Class 1 and Class 2 Fistulae Procedures 100% 18 80% Percent Patent 16 60% 14 Diameter (mm) 12 40% 10 pre BAM 20% 8 post BAM 6 0% 4 0 6 12 18 24 30 36 2 Time (Months) 0 (months) Class 1 Primary Patency Class 2 Primary Patency Class 1 Secondary Patency Class 2 Secondary Patency Annual Mortality Rate (20%) Class 1 Class 2 AVF Technical Success w/o AVF Failure Clinical Success AVF Technical and Clinical Success 1
ASDIN 7th Annual Scientific Meeting Based on 2007 ERSD data At just under $60,000 $60,000 , PPPY costs for patients with an AV FISTULA FISTULA are 18-25% lower than those for patients with a catheter or graft. Based on 2007 ERSD data, the annual cost per patient is: $75,344 ($6278.66/mo) for a Catheter (7%) ACCESS EVENT costs are $5,960 & $7,451 per person per year for ACCESS EVENT patients with a catheter or AV graft, compared to $3,194 for those with an AV fistula. $72 729 ($6060 75/ $72,729 ($6060.75/mo) for a AV Graft (15%) ) f AV G ft (15%) $55,112 ($4592.66/mo) for a AV Fistula (4%) Costs for vascular access services performed by nephrologists continue to rise, &, at $19 PPPY in 2007, were nearly 10 TIMES 10 TIMES greater than in 2000. Secondary Patency Study Mean AVF age, Treatment 3-mon. 6-mon. 12-mon. 24-mon. 36-mon. n range(months) Turmel- PTA only Rodrigues ’01 2.6 52 88% 83% 79% 75% N/A (1–6.5 ) Beathard ’99 PTA +/ − 5 Sg occl 63 82.5% 78% 74.7% (1.1–14 ) Nassar ’06 PTA +/ − Sg occl 8.9 119 100% 100% 95% N/A N/A (3-14.8 ) Falk ’06 PTA +/ − Sg occl 65 10.6 (0.4-38 ) 73% 72% 68% Miller ‘09 Class 1 39 96% 96% 92% 53% 42% 25 PTA, coil occl, Miller ‘09 (0.25–44 ) LiCE, Fr Class 2 58 94% 91% 76% 61% 32% • Flow Rerouting with Elimination of Techniques Competing Branch Veins Thrombectomy Maturation • Staged Sequential Dilation • Long Length Balloon PTA Step1: Find the Anastamosis • Limited Controlled Extravasation Directional Guidance Rotate Guiding Catheter 2
ASDIN 7th Annual Scientific Meeting Wire Guided Flow Rerouting Confirm Basilic Outflow Vein Wire Guided Selective Demonstrate Basilic Vein Pathway Catheterization Confirm Lumen Find Point of Greatest Stenosis using 0.018 Guiding Catheter Dilate in 1mm Increments until 6mm Retrograde Access Using Balloon using Long Length Balloons Puncture Technique Fully Efface all Stenoses and Dilate Inflow Stenosis Restore Flow Eliminate Problematic Collateral Veins Restore Flow / Troubleshoot Forearm Flow / Check for Upper Arm Flow / Check for Perforations Unimpeded Drainage Retrogr Retrograde Colla Collate terals Ante Antegrade Colla llaterals 3
ASDIN 7th Annual Scientific Meeting Dilate Using Final Inspection Inflow Control • Using Manual Pressure at the anastamosis • Protect torn distal vein segments from arterial inflow pressure during re ‐ angioplasty of proximal segments • Avoid exposing injured distal segments to high arterial pressure during periods of balloon occlusion Before 2 nd Ballooning Follow ‐ up at 2 weeks Follow ‐ up at 4 Weeks After 2 nd Ballooning Things don’t always go so well….. g y g Sometimes BAM = BOOM 4
ASDIN 7th Annual Scientific Meeting Sal Salvage the e the Sal Salvage Pro Proced edure - prolonged angioplasty Figure 1: Patient attrition flowchart. - stent placement Age – Mean, Range (years) 63.6 (17 ‐ 88) Table 2: Thrombectomy Statistics for 108 Fistulas Table 1: Patient Demographics Male gender (%) 67 Diabetes mellitus (%) 61 BBF BCF FF Hypertension (%) 91 ( n = 24) ( n = 29) ( n = 55) Fistula Type, n (%) Percentage of Fistulas Requiring Radial ‐ cephalic 69 (49) 24% 2% 3% Arterial Angioplasty Brachial ‐ cephalic 39 (28) Percentage of Fistulas Requiring Percentage of Fistulas Requiring Brachial ‐ basilic 4 (3) 4% 21% 54% Angioplasty of the Anastomosis Brachial ‐ transposed basilic 26 (19) Brachial ‐ antecubital 1 (1) Percentage of Fistulas With Ulnar ‐ basilic 1 (1) Venous Perforation or Elastic 33% 21% 2% Average fistula age at time of first intervention (months) 5.6 Recoil Requiring Stent Placement Thrombosis Duration – Mean, Range (weeks) Abbreviations Used: AVF=arteriovenous fistula, 3 (1 ‐ 12) BBF=brachiobasilic fistula, BCF=brachiocephalic fistula, Average Midbody Fistula Diameter Prior to Initial ntervention 1.5mm FF=forearm fistula Length of Thrombosed Vein Segment – Mean, Range (cm) 15 (5 ‐ 35 ) Figure 3: Primary Assisted Patencies of Forearm, Brachial ‐ basilic, and Brachial ‐ cephalic Figure 2: Primary Access Patencies of Forearm, Brachial ‐ basilic, and Brachial ‐ cephalic Fistulas Fistulas 5
ASDIN 7th Annual Scientific Meeting Figure 4: Secondary Access Patencies of Brachial ‐ basilic, Brachial ‐ cephalic, and Table 3: Follow ‐ Up Statistics for 108 Matured Fistulas Forearm Fistulas Time All AVFs BBF BCF FF (Months) ( n = 108) ( n = 24) ( n = 29) ( n = 55) Primary Access 3 54% 50% 40% 63% Patency 6 29% 13% 22% 41% Primary Assisted 6 78% 73% 77% 80% Patency 12 59% 49% 52% 66% Secondary Access 12 90% 95% 84% 92% Patency 24 80% 95% 74% 79% Post ‐ Maturation Interventions Per 2.78 3.56 3.46 2.03 Access ‐ year Post ‐ Maturation Thrombectomies 0.52 0.64 0.72 0.35 Per Access ‐ year Abbreviations Used: AVF=arteriovenous fistula, BBF=brachiobasilic fistula, BCF=brachiocephalic fistula, FF=forearm fistula What does it COST ? Cost calculations: Percutaneous salvage: New access placement (assuming maturation time of 3 months): New access placement (assuming maturation time of 9 months): $12,904 = cost of maturation process based on presented data and Medicare reimbursement rates + $9,496 = cost of 46 days of catheter use during average maturation period + $48,166 = [ (365 − 46 days of fistula use) ÷ 365] × ($55,112 per patient per year cost of fistula) $70,566 = total cost per patient for the first year following the initial referral for the percutaneous route $15,359 = cost of surgery + $18,836 = cost of 3 months of catheter usage according to USRDS data + $41,334 = cost of 9 months of fistula usage according to USRDS data $75,529 = total cost per patient for the first year following the initial referral for the surgical route $15,359 = cost of surgery + $56,509 = cost of 9 months of catheter usage according to USRDS data + $13,778 = cost of 3 months of fistula usage according to USRDS data $85,646 = total cost per patient for the first year following the initial referral for the surgical route CONCLUSION: Thrombectomy At just under $60,000 $60,000 , PPPY costs for patients with an AV FISTULA FISTULA Maturation are 18-25% lower than those for patients with a catheter or graft. • Thrombectomy Maturation – Allows for the use of suboptimal veins – Dilation of the vein results in full thickness rupture of ACCESS EVENT ACCESS EVENT costs are $5,960 & $7,451 per person per year for the vein wall, allowing primarily pressure to continue patients with a catheter or AV graft, compared to $3,194 for those the dilation process the dilation process with an AV fistula. – As long as elevated flow and pressure are present, in the absence of competing branch veins, the AVF will dilate rather than sclerose. Costs for vascular access services performed by nephrologists – 99/148 AVF’s functioning at 12 months. continue to rise, &, at $19 PPPY in 2007, were nearly 10 TIMES 10 TIMES greater than in 2000. – Results in significant cost savings over abandonment and revision (even in best case abandonment scenario). 6
Recommend
More recommend