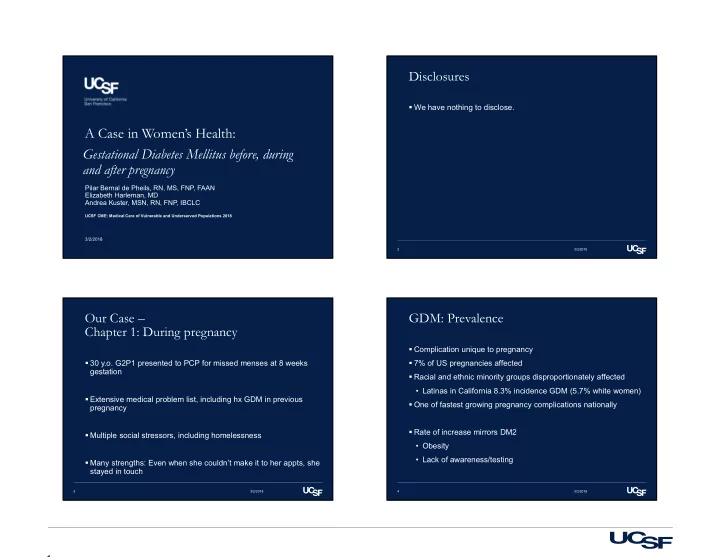
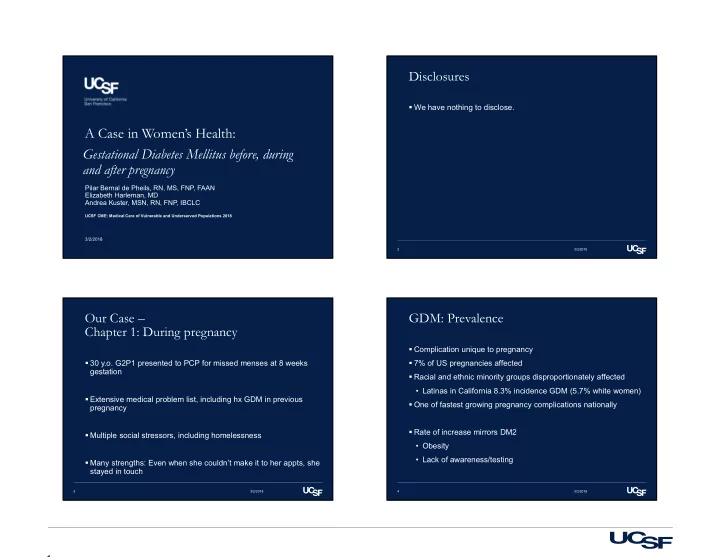
Disclosures We have nothing to disclose. A Case in Women’s Health: Gestational Diabetes Mellitus before, during and after pregnancy Pilar Bernal de Pheils, RN, MS, FNP, FAAN Elizabeth Harleman, MD Andrea Kuster, MSN, RN, FNP, IBCLC UCSF CME: Medical Care of Vulnerable and Underserved Populations 2018 3/2/2018 2 3/2/2018 Our Case – GDM: Prevalence Chapter 1: During pregnancy Complication unique to pregnancy 30 y.o. G2P1 presented to PCP for missed menses at 8 weeks 7% of US pregnancies affected gestation Racial and ethnic minority groups disproportionately affected • Latinas in California 8.3% incidence GDM (5.7% white women) Extensive medical problem list, including hx GDM in previous One of fastest growing pregnancy complications nationally pregnancy Rate of increase mirrors DM2 Multiple social stressors, including homelessness • Obesity • Lack of awareness/testing Many strengths: Even when she couldn’t make it to her appts, she stayed in touch 3 3/2/2018 4 3/2/2018 1
GDM: Risks Diagnostic and Management Considerations In pregnancy Diagnostic and management considerations • Macrosomia/Shoulder dystocia/Birth injury • Who do we test for GDM? • Neonatal hypoglycemia • When do we test? • C-section delivery • What diagnostics we utilize? • Hypertensive disorders (i.e. preeclampsia) After pregnancy • Mom: increased risk (50-70%) of developing DM2 • Baby: increased risk of DM2 5 3/2/2018 6 3/2/2018 Who is at risk for GDM? Gestational Diabetes: When do we test? First-degree relative with diabetes Test for undiagnosed diabetes at the first prenatal visit in those with risk factors, using standard High-risk race/ethnicity (e.g., AA, Latino, NA, Asian A, PI) diagnostic criteria. B History of GDM or pre-diabetes, stillbirth or fetal malformation Test for gestational diabetes mellitus at 24–28 Women with PCOS, Htn, HLD, CVD weeks of gestation in pregnant women not Other clinical conditions associated with insulin resistance (e.g., previously known to have diabetes. A overweight or obesity, chronic steroid or atypical antipsychotic use, acanthosis nigricans). Physical inactivity 7 3/2/2018 8 3/2/2018 2
Screening for DM: How do we test? How Do We Manage GDM? Initial OB Visit Lifestyle change is an essential component of management of gestational diabetes mellitus and may suffice for the treatment for Routine: HgA 1C many women. Medications should be added if needed to achieve glycemic targets. A At risk: Add FBS • HgA1C ≥ 5.7% FBS <92 GTT Insulin is the preferred medication for treating hyperglycemia in • FBS≥ 92 ANY Hg A1C Pre-existing pre-gestational diabetes gestational diabetes mellitus, as it does not cross the placenta to a measurable extent. Metformin and glyburide may be used, but both Routine (24 to 28 W) cross the placenta to the fetus, with metformin likely crossing to a “One-step” 75-g OGTT or greater extent than glyburide. All oral agents lack long-term safety data. A 2. “Two-step” approach with a 50-g (nonfasting) screen followed by a 100-g OGTT for those who screen positive 9 3/2/2018 10 3/2/2018 How Do We Manage GDM? Clinical Pearls from our case Metformin, when used to treat polycystic ovary syndrome and Back to our patient and her barriers: induce ovulation, need not be continued once pregnancy has been • Challenges with screening confirmed. A • Obstacles to care ‒ Cultural/religion Fasting and postprandial self-monitoring of blood glucose are recommended in both gestational diabetes mellitus and preexisting ‒ Housing and transportation diabetes in pregnancy to achieve glycemic control. B Strengths supporting her care • Patient Centered Care ‒ Continuity of care ‒ Clinic resources/CA State supported resources in pregnancy ‒ Support based on her values/respectful of her decisions 11 3/2/2018 12 3/2/2018 3
Our Case – Clinical Pearls: Chapter 2: After the birth Start Education and Planning during Pregnancy - Don’t Wait until Post-Partum! Returns to PCP at 2-3 months post-partum (didn’t f/u with OB) • Post-partum GTT was ordered by L&D, not done yet GDM and life-long risk • Breastfeeding frequently, mostly at night, and mom feeding formula • Preview post-partum f/u, importance of weight management during the day through diet and exercise, and annual f/u with PCP including A1c • Desires Mirena IUD Contraception • Know the plan before the birth! What are your priorities? Breastfeeding • Emphasize additional benefits for mom and baby 13 3/2/2018 14 3/2/2018 Our Case – Chapter 3: Contemplating another pregnancy If you take care of women of reproductive Patient returns to you two years later, contemplating third pregnancy age, it’s not a question of whether you provide preconception care, rather it’s a What pre-conception counseling would you do? question of what kind of preconception care you are providing. Joseph Stanford 15 3/2/2018 16 3/2/2018 4
Preconception Care for All Preconception in Diabetes Assess risk Starting at puberty, preconception counseling should be incorporated into routine diabetes care for all girls of • Health, pregnancy intention, contraception childbearing potential. A Give protection Family planning should be discussed and effective • Folic acid, immunizations contraception should be prescribed and used until a woman is prepared and ready to become pregnant. A Manage conditions • Diabetes, obesity, hypothyroidism, STI Preconception counseling should address the importance of glycemic control as close to normal as is safely possible, Avoid harmful exposures ideally A1C 6.0-6.5%, to reduce the risk of pregnancy loss • Medications, alcohol, tobacco and congenital anomalies. B 17 3/2/2018 18 3/2/2018 Preconception Case continued Women with preexisting type 1 or type 2 diabetes You send a HgBA1C to aid in preconception counseling who are planning pregnancy or who have become It returns at 8.2% pregnant should be counseled on the risk of development and/or progression of diabetic retinopathy. Dilated eye examinations should occur before pregnancy or in the first trimester, and then patients should be monitored every trimester and for 1 year postpartum as indicated by degree of retinopathy and as recommended by the eye care provider. B 19 3/2/2018 20 3/2/2018 5
Clinical Pearl Case continued Never (almost never) tell a woman with a medical illness she After counseling about the risks of birth defects and pregnancy shouldn’t get pregnant. loss, your patient decides to use contraception until getting her newly diagnosed DM under better control What are her options for contraception? 21 3/2/2018 22 3/2/2018 U.S. MEC: Categories Example: Smoking and Contraceptive Use No restriction for the use of the contraceptive method 1 for a woman with that condition Advantages of using the method generally outweigh 2 the theoretical or proven risks Theoretical or proven risks of the method usually outweigh the advantages – not usually recommended 3 unless more appropriate methods are not available or acceptable Unacceptable health risk if the contraceptive method 4 is used by a woman with that condition Cu IUD: Copper IUD; LNG-IUD: Levonorgestrel IUD; DMPA: Depo-Medroxyprogesterone Acetate; POPs: Progestin-only pills; CHCs: Combined hormonal contraceptives including pills, patch, and ring 6
Diabetes and Contraception § This condition is associated with increased risk for adverse health events as a result of pregnancy † This category should be assessed according to the severity of the condition 26 3/2/2018 Importance of screening for SDH: Importance of screening for SDH: TAILORING TREATMENT TO REDUCE DISPARITIES TAILORING TREATMENT TO REDUCE DISPARITIES Providers should assess social context, including Treatment plans should align with the Chronic Care potential food insecurity, housing stability, and Model, emphasizing productive interactions between financial barriers, and apply that information to a prepared proactive practice team and an informed treatment decisions. A activated patient. A Patients should be referred to local community When feasible, care systems should support team- resources when available. B based care, community involvement, patient registries, and decision support tools to meet patient needs. B Patients should be provided with self-management support from lay health coaches, navigators, or community health workers when available. A 27 3/2/2018 28 3/2/2018 7
Recommend
More recommend